Most people know there are two types of diabetes—type 1 and type 2. Knowing which one you have matters quite a lot for how you treat them. But what you may not know about is a lesser-known variation of the disease: latent autoimmune diabetes in adults (LADA), sometimes referred to informally as type 1.5 diabetes.
Often mistaken for type 2 diabetes due to its slow onset in adulthood, LADA is, in fact, an autoimmune disease, more closely related to type 1. Its symptoms don’t quite fit the mold of type 1 or type 2 diabetes—yet these distinctions are frequently missed, leading to delayed or ineffective treatment that could result in health complications down the line.
But scientists are starting to tease out a better understanding of what causes this form of diabetes and how to distinguish its symptoms. Here’s what endocrinologists want you to know—and their tips on advocating for proper testing and a diagnosis.
What is LADA?
All three types of diabetes belong under the umbrella of diabetes mellitus—a disorder characterized by elevated blood sugar, the body’s main source of energy. This can happen for a variety of reasons, explains Alexander Turchin, endocrinologist with Mass General Brigham, mainly related to insulin, a hormone that plays a key role in regulating blood sugar levels.
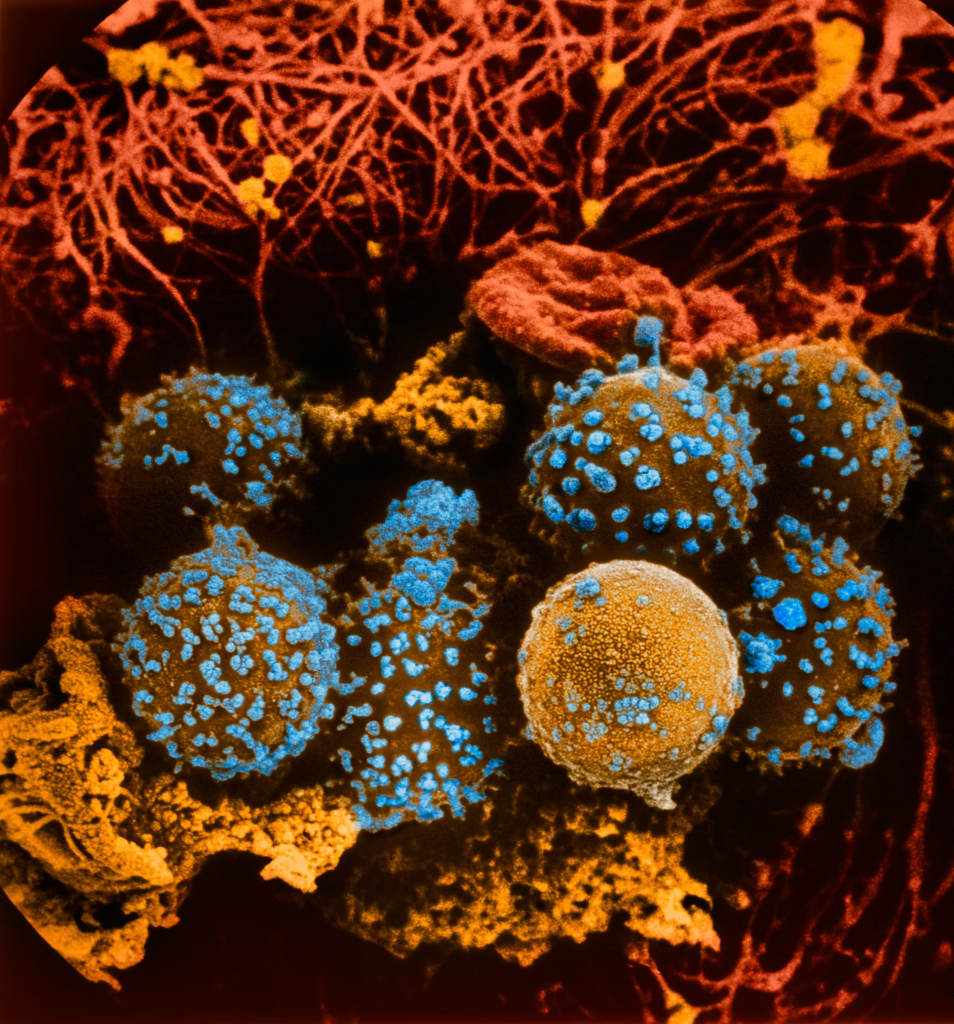
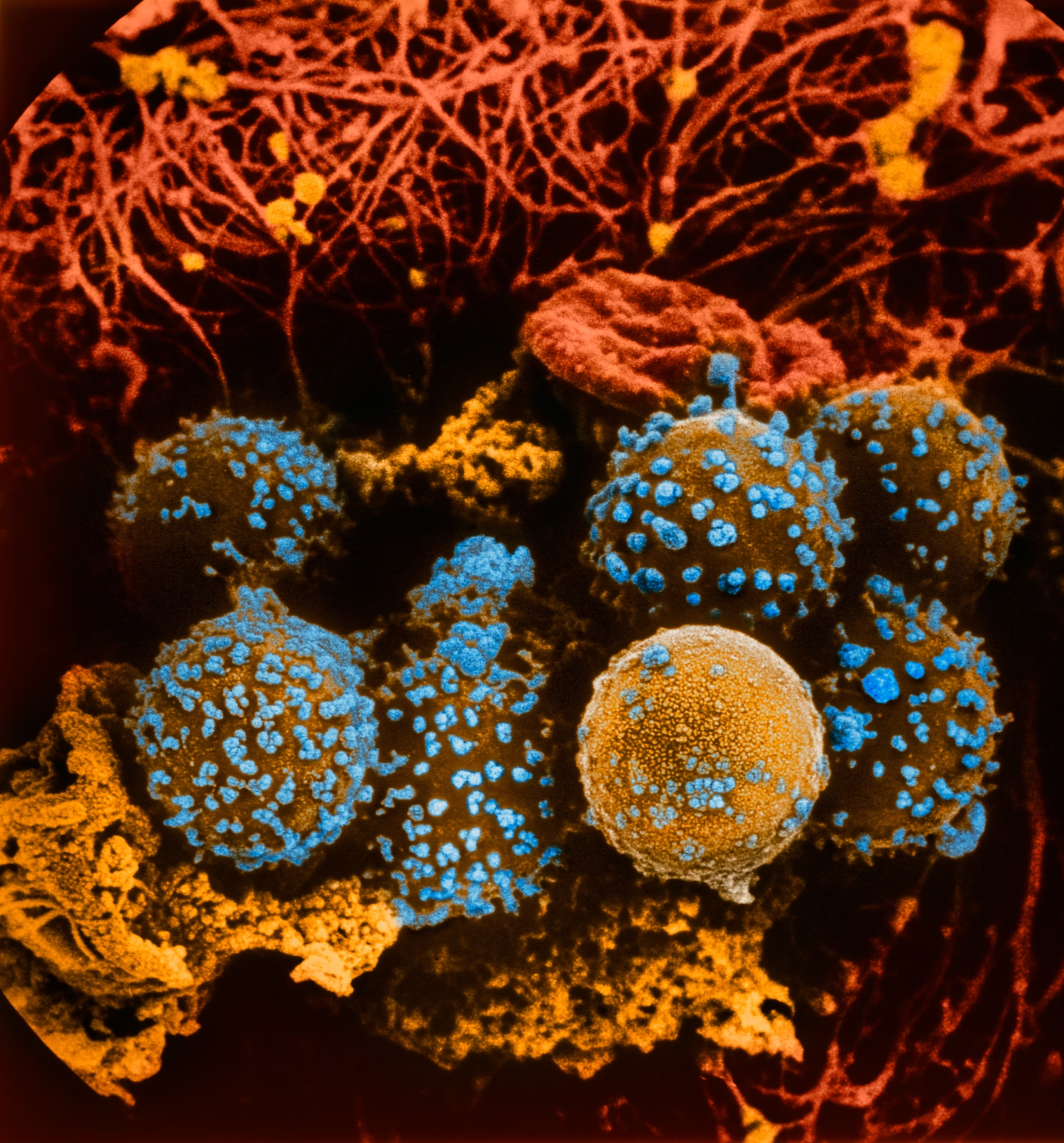
Type 1 diabetes occurs when the pancreas doesn’t make enough insulin, Turchin says. This is an autoimmune disease in which antibodies in the immune system go rogue and destroy the specific cells in the pancreas that make insulin. As time goes on, there are too few cells and not enough (or no) insulin is made. Genetics play a key role in type 1 diabetes, which is most commonly diagnosed in children and young adults.
Type 2 diabetes occurs when your body isn’t sensitive enough to insulin—also known as insulin resistance, according to Turchin. “In other words, there is plenty of insulin, but the body doesn’t react to it the way it should,” Turchin says. As a result, “sugar can’t be tolerated.” While genetics can play a role, lifestyle factors like being overweight or not getting enough exercise are typically behind it as they can expose your body to too much blood sugar over an extended period of time. People of any age can get type 2 diabetes but it is often diagnosed in those 45 or older, according to the U.S. Centers of Disease Control and Prevention (CDC).
(How eating too much sugar as a child impacts you for life.)
LADA similarly tends to appear in older individuals—typically around age 30 or older—but that’s because this version of the disease progresses in a slow burn compared to type 1 diabetes.
People develop classic symptoms, like frequent urination and thirst, and rapid weight loss, over a period of days or weeks. “When these symptoms occur, the autoimmune process has been going on for a while, but it finally reached the stage where really the body cannot compensate anymore and the blood sugar starts rising quickly,” Turchin says.
With LADA this process happens more slowly. “It’s the same mechanism, but instead of happening over, say, two weeks, it happens over years,” Turchin says. “It’s the same antibodies against the same cells in the pancreas, but they’re just working more slowly and [the patient’s] insulin levels are dropping more slowly and their blood sugar is rising more slowly.”
Like type 1 diabetes, there’s a genetic component to LADA, but there may also be environmental components at play, like lower respiratory infections, according to a research article in Diabetes/Metabolism Research and Reviews. And the condition isn’t nearly as common—it accounts for about 2 to 12 percent of all people diagnosed with diabetes as adults, according to the American Diabetes Association.
Why is LADA often misdiagnosed?
Symptoms of LADA are extremely similar to those of type 1 and type 2 and include unexplained weight loss, excessive thirst, excessive urination, increases in infections, and skin lesions that won’t heal, says Schafer Boeder, endocrinologist with UC San Diego Health.
“Misdiagnosis is a big problem in LADA,” Boeder says.
About 5 to 10 percent of LADA cases are misdiagnosed. That’s in part because of the symptom overlap but also it may be due to the misconception that autoimmune diabetes, like type 1 diabetes, can only occur in children and adolescents, Boeder adds.
(Why women are more prone to autoimmune diseases.)
“In those cases, generally people are doing what they’re being asked to do by their provider—they’re working on their diet, they’re trying to increase their physical activity, they’re taking their medications that are being prescribed. But none of this is effective,” Boeder says. “Instead, they’re seeing a rapid rise in their blood sugar despite the appropriate lifestyle changes and medications. That’s when LADA sort of starts to differentiate itself from type 2 diabetes.”
Because the first line of intervention for type 2 diabetes is making lifestyle changes, people diagnosed with the condition those patients don’t necessarily need insulin injections right away. However, people with LADA do need insulin —sooner than people with type 2 diabetes and, so a delay in treatment can be dangerous, explains Kathleen Dungan, an endocrinologist with The Ohio State University Wexner Medical Center.
If someone’s LADA goes undiagnosed for even five to 10 years, they could develop diabetic ketoacidosis and possibly die if not treated adequately, adds Kathleen Wyne, also an endocrinologist with The Ohio State University Wexner Medical Center. This condition occurs due to uncontrolled blood sugar and/or missing doses of medication for prolonged periods of time. When your insulin is continuously too low, your body breaks down fat too quickly and processes this fat into a fuel called ketones. The result? Acidic blood, which can be fatal if not treated quickly.
How to advocate for a diagnosis
Getting to a LADA diagnosis is difficult for both a patient and their doctor, Boeder says.
“The patient often goes through a misdiagnosis or a period of not knowing what’s going on, and that can be frustrating,” he says. “And likewise for the provider, sometimes misdiagnosis comes down to a lack of awareness about the fact that adults can have autoimmune diabetes. But also, a lot of times it’s just a difficult diagnosis to make, especially early on.”
If you’ve been diagnosed with type 2 diabetes but aren’t responding to treatment, it’s a good idea to bring up LADA with your doctor, Boeder says.
You’ll need to ask your diabetes team (usually your primary care clinic) to screen you for type 1 diabetes, according to Wyne. “Most adult clinics do not know how to do this,” she says. “The important thing is to have them draw the five antibodies—GAD, ICA, IAA, IA2, and ZnT8. Just measuring glucose, or A1c, or c-peptide—or any combination of those three—is not adequate.” If these antibodies are positive, it “very strongly supports” the case that this is LADA diabetes, Boeder adds.
LADA can be very effectively treated once the diagnosis is made, Boeder says. It’s all about working with your care team to monitor how much insulin you need and when in the form of an insulin pen or pump, which can connect to continuous glucose monitors to manage your blood sugar at all times. In some cases, GLP-1 agonist drugs, such as Ozempic and Wegovy, may work.
If your LADA is well controlled, you can live a “long and healthy life that’s just as long—or even longer—than people who don’t have diabetes,” Boeder says.
发表回复